Diabetes mellitus, a chronic condition characterized by high blood sugar levels, casts a long shadow across the globe. According to the International Diabetes Federation (IDF), over 537 million adults were living with diabetes in 2021, with projections estimating a staggering 783 million by 2045. This alarming prevalence underscores the critical need for advancements in diabetes treatment and management. Fortunately, the field of diabetes research is brimming with exciting developments, offering hope for a sweeter future for millions.
1. The urgent need for innovation
Diabetes, particularly type 2 diabetes, has become a global health crisis. It is a leading cause of blindness, kidney failure, heart disease, stroke, and lower limb amputation. The economic burden is equally concerning, with the International Diabetes Federation (IDF) estimating the global cost of diabetes at US$966 billion in 2021. Despite these alarming statistics, a wave of innovation is transforming the diabetes treatment landscape, offering both improved management strategies for existing patients and potential cures for the future.
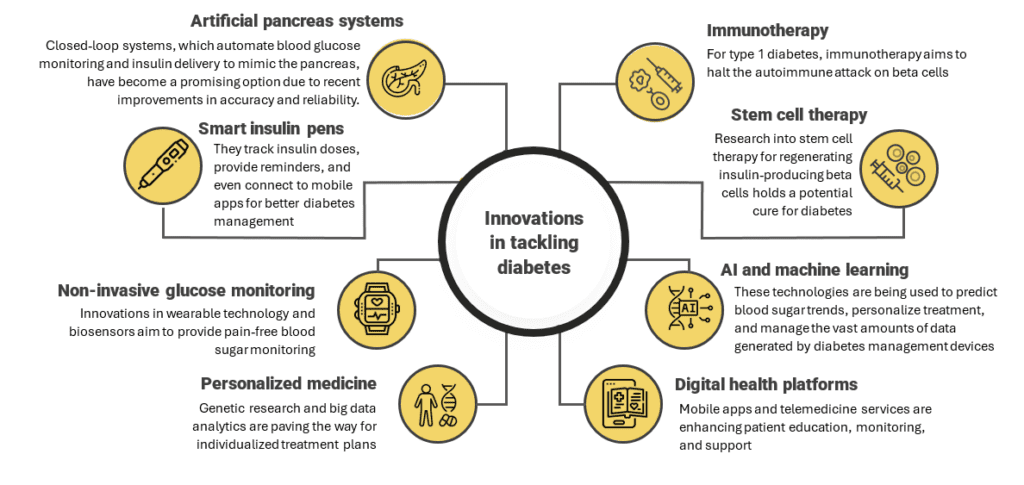
The following are the innovations in tackling diabetes and improving the patient’s quality of life:
2. Current standard treatments and their limitations
For type 1 diabetes, insulin therapy via multiple daily injections or continuous subcutaneous insulin infusion (CSII) with an insulin pump is the standard. This requires constant monitoring and adjustment to maintain optimal blood glucose levels.
For type 2 diabetes, initial treatment typically includes lifestyle modifications and oral medications like metformin. As the disease progresses, additional medications, including injectables like GLP-1 agonists and insulin, may be required.
- Lifestyle modifications: Dietary changes, regular physical activity, and weight management. Challenges include busy schedules, lack of motivation, social influences, and weight loss plateaus
- Oral medications: Metformin, sulfonylureas, and SGLT2 inhibitors manage blood glucose but may cause gastrointestinal issues, hypoglycemia, weight gain, and infections. Their effectiveness can decrease over time, often requiring insulin or additional medications
- Insulin therapy: Essential for type 1 and advanced type 2 diabetes, using basal and bolus insulin. Risks include hypoglycemia and weight gain, requiring regular follow-ups for dose adjustments
- Continuous Glucose Monitors (CGMs): Provide real-time blood glucose readings for precise insulin dosing. They may give inaccurate readings during rapid glucose changes and require frequent sensor replacements
- Insulin pumps: Deliver continuous insulin through a catheter, reducing the need for multiple daily injections. They are expensive, require regular maintenance, and may not be fully covered by insurance.
3. Advances in treatment options for type 1 diabetes
3.1. Insulin therapies
3.1.1. Modern insulin formulations
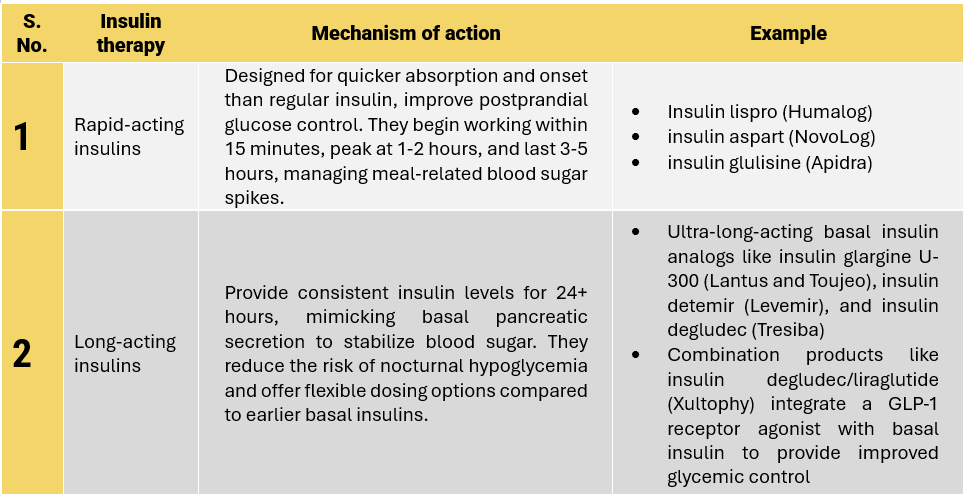
Advances in the treatment options for type 1 diabetes have significantly improved the management of the disease, enhancing the quality of life for individuals affected by it. The development of rapid-acting insulins and long-acting insulins are some of the key areas of progress in insulin therapy.
Modern insulin formulations and their mode of action:
3.1.2. Advances in insulin delivery methods
Type 1 diabetes management has seen remarkable progress with the advent of advanced insulin delivery methods. These innovations have significantly enhanced the precision, convenience, and effectiveness of insulin therapy, improving the quality of life for individuals with Type 1 diabetes.
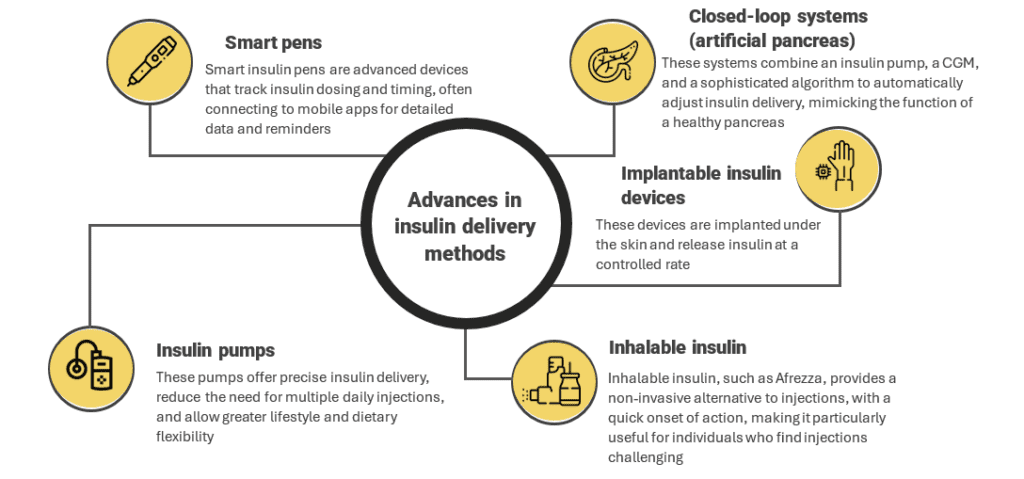
Recent advances in insulin formulations and delivery methods have significantly improved the management of type 1 diabetes. Rapid-acting and ultra-long-acting insulins, combination products, insulin pumps, and closed-loop systems have all contributed to better glycemic control and reduced risk of complications for patients. However, challenges remain in terms of cost, access, and the burden of diabetes management.
3.2. Emerging therapies and technologies
Ongoing research aims to develop alternative type 1 diabetes treatment approaches like artificial pancreas systems, immune modulation therapies, and cell-based therapies.
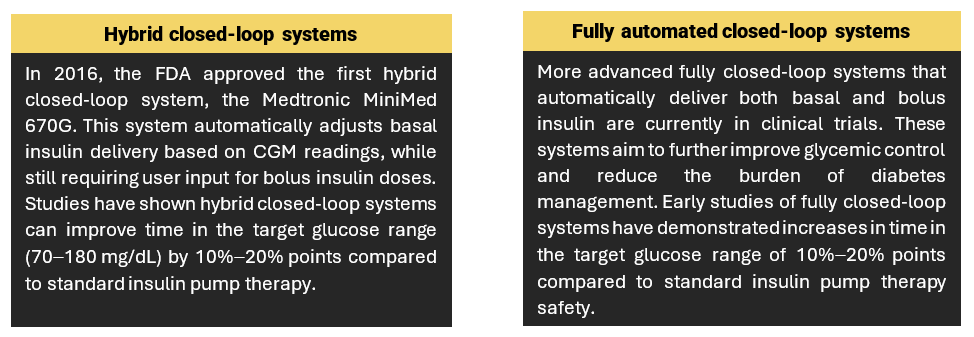
3.2.1. Artificial pancreas systems
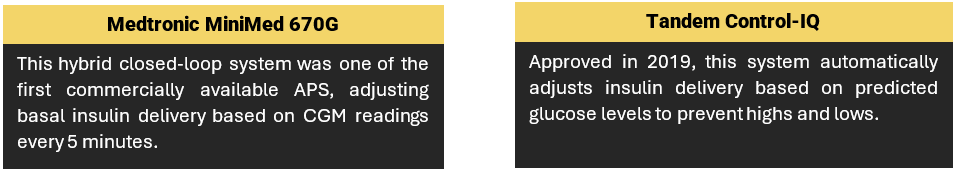
The development of closed-loop artificial pancreas systems has made significant progress in recent years. These systems integrate CGM with an insulin pump to automatically adjust insulin delivery based on real-time glucose levels, without requiring user input.
Key milestones:
Latest approved devices:
Investigational devices in clinical trials:
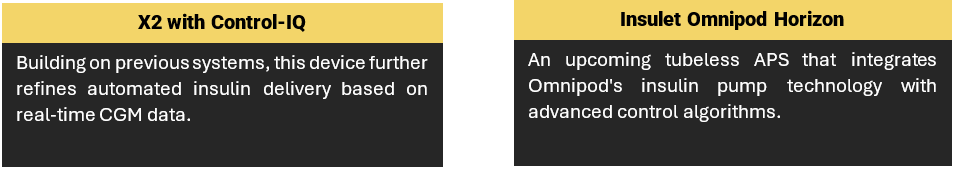
- Other investigational devices that are in clinical trial are Medtronic advanced hybrid closed-loop, Beta Bionics iLet bionic pancreas, and Inreda dual-chamber artificial pancreas
These experimental systems have demonstrated encouraging outcomes in clinical trials, including increased time spent within the target glucose range and decreased occurrences of hypoglycemia when compared to conventional insulin pump therapy. Continued research endeavors seek to enhance artificial pancreas technologies further and broaden access for individuals with type 1 diabetes.
3.2.2. Immune modulation therapies
Immune modulation therapies represent a promising frontier in type 1 diabetes research, aiming to halt or reverse the autoimmune destruction of insulin-producing beta cells in the pancreas. These therapies focus on modifying the immune response to preserve remaining beta-cell function or restore insulin production.
Significant progress has been made in developing immune modulation therapies to preserve or restore beta-cell function in type 1 diabetes.
- Antigen-specific immunotherapies: These therapies aim to induce immune tolerance by targeting specific autoantigens involved in the autoimmune destruction of beta cells
Examples:
- Peptide immunotherapy (Teplizumab) showed preservation of C-peptide levels and reduced insulin requirements in recent-onset type 1 diabetes patients in clinical trials
- GAD-alum (Diamyd) demonstrated preservation of beta-cell function in some recent-onset type 1 diabetes patients in phase 2 trials.
Key studies and clinical trials:
- The Phase 3 TN-10 trial of teplizumab (ClinicalTrials.gov number: NCT01030861) in high-risk individuals showed a median delay in onset of type 1 diabetes by nearly 3 years compared to placebo
- The Phase 2 DiAPREV-IT 2 trial of GAD-alum (ClinicalTrials.gov number: NCT01122446) in recent-onset type 1 diabetes patients found a significant increase in the proportion of participants with preserved beta-cell function at 15 months
- Broad immune modulators: These therapies aim to broadly suppress or regulate the autoimmune response without targeting specific antigens
Examples:
- Anti-CD3 monoclonal antibodies (Teplizumab and Otelixizumab) delayed progression to type 1 diabetes in high-risk individuals and preserved beta-cell function in recent-onset patients in clinical trials
- CTLA-4-Ig (Abatacept) preserved beta-cell function in new-onset type 1 diabetes patients in a phase 2 trial
Key studies and clinical trials:
- The Phase 2 AbATE trial of abatacept (ClinicalTrials.gov number: NCT00505375) in new-onset type 1 diabetes patients demonstrated a significant increase in C-peptide levels and reduced insulin requirements at 2 years
- The Phase 3 DEFEND-1 trial of otelixizumab (ClinicalTrials.gov number: NCT00678886) in recent-onset type 1 diabetes patients showed a modest preservation of beta-cell function, but the trial did not meet its primary endpoint
Immune modulation therapies represent a dynamic area of research in type 1 diabetes treatment, offering hope for slowing disease progression and potentially achieving disease remission through preservation or restoration of beta-cell function. Continued advancements in understanding immune mechanisms and refining therapeutic approaches hold promise for transforming the management and outlook of type 1 diabetes in the future.
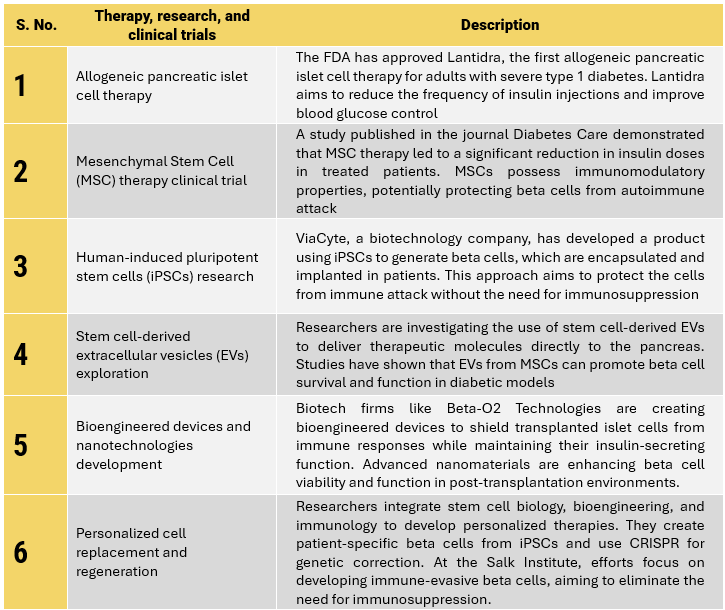
3.2.3. Cell-based therapies
Research is ongoing into the use of stem cells to develop insulin-producing beta cells that can be transplanted into patients. Cell-based therapies for type 1 diabetes have made significant advances in recent years, driven by innovations in stem cell research and beta-cell transplantation.
- Stem cell-derived beta cells (sBCs) production faces cost and labor challenges for achieving mature, functional cells and eliminating tumor-causing stem cell remnants, limiting scalability
- University of Florida researchers use chemotherapeutic drugs to selectively remove non-beta cells from sBC cultures, enhancing maturation and functionality while reducing production costs and time
- Islet cell transplantation from donor pancreases into the livers of type 1 diabetes patients can produce insulin, potentially reducing or eliminating the need for insulin injections, though challenges include donor scarcity and lifelong immunosuppression needs to prevent rejection
Notable research and emerging treatments in cell-based therapies:
4. Advances in treatment options for type 2 diabetes
Managing type 2 diabetes involves a multifaceted approach, including medications, surgical interventions, and lifestyle modifications. Recent advancements have significantly expanded the treatment arsenal, providing more effective and personalized options for patients.
4.1. Oral medications
New class of oral hypoglycemic agents:
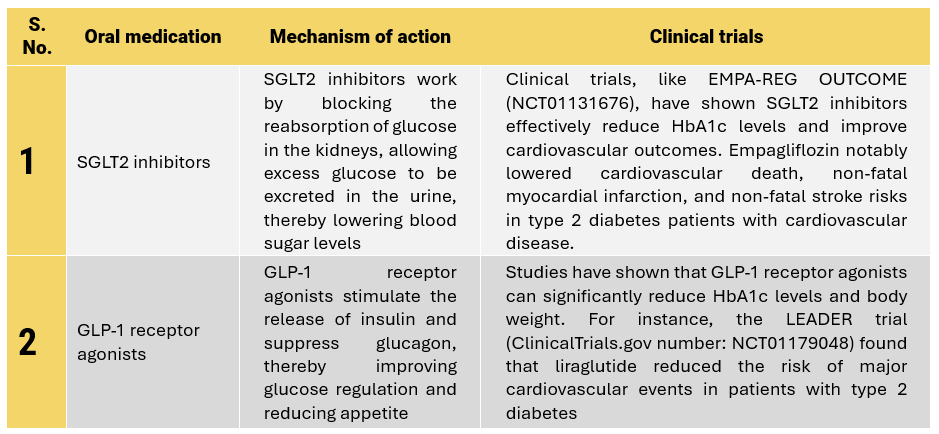
Combining SGLT2 inhibitors and GLP-1 receptor agonists offers added benefits over monotherapy. A large retrospective cohort study (Clinical trial number: 268-OR) with over two million type 2 diabetes patients showed this combination significantly reduces all-cause mortality, myocardial infarction rates, and hospital admissions compared to monotherapy.
In a real-world setting, the combination therapy showed a hazard ratio (HR) of 0.25 for all-cause mortality, 0.60 for hospital admissions, and 0.63 for myocardial infarction rates, indicating a substantial improvement in cardiovascular outcomes.
4.2. Non-insulin injectables
GLP-1 receptor agonists enhance glucose-dependent insulin secretion, slow gastric emptying, and reduce postprandial glucagon levels. Examples include liraglutide, semaglutide, and dulaglutide, which significantly reduce HbA1c and body weight. The LEADER trial showed liraglutide also reduces major cardiovascular events in type 2 diabetes patients.
Dual GLP-1 and GIP receptor agonists, or “twincretins,” are a significant advancement in type 2 diabetes treatment. These agents enhance insulin secretion and improve glucose regulation by activating both GLP-1 and GIP receptors. They provide better glycemic control, greater weight loss, and cardiovascular and renal benefits compared to single GLP-1 receptor agonists. For example, tirzepatide more effectively reduces HbA1c than other GLP-1 receptor agonists.
Current studies on dual GLP-1 and GIP receptor agonists include:
The SURPASS-CVOT study is currently assessing the cardiovascular protective effects of tirzepatide compared to dulaglutide.
The SURMOUNT program is exploring the use of tirzepatide for the treatment of obesity and metabolic-associated fatty liver disease (MAFLD).
4.3. Bariatric surgery
Bariatric surgery effectively manages type 2 diabetes in obese patients by improving insulin sensitivity and beta-cell function. It induces hormonal changes, increases GLP-1 levels, enhances insulin secretion, promotes satiety, and leads to significant weight loss and better glycemic control, potentially achieving diabetes remission.
Key points supporting the effectiveness include:
- Studies have indicated that up to 80% of patients achieve diabetes remission within the first two years post-surgery
- Longitudinal studies have demonstrated sustained diabetes remission and improvement in glycemic control for many years following surgery. The Swedish Obese Subjects (SOS) study found that 10 years post-surgery, approximately 36% of patients remained in remission
- A landmark study published in the New England Journal of Medicine demonstrated that surgical patients had better glycemic outcomes than those receiving intensive medical therapy
- A large meta-analysis found that 66.7% of patients achieved type 2 diabetes remission after bariatric surgery, compared to only 6.3% with non-surgical treatment
- The remission rates are highest with procedures like Roux-en-Y gastric bypass (up to 80%–90%) and sleeve gastrectomy (60%–70%)
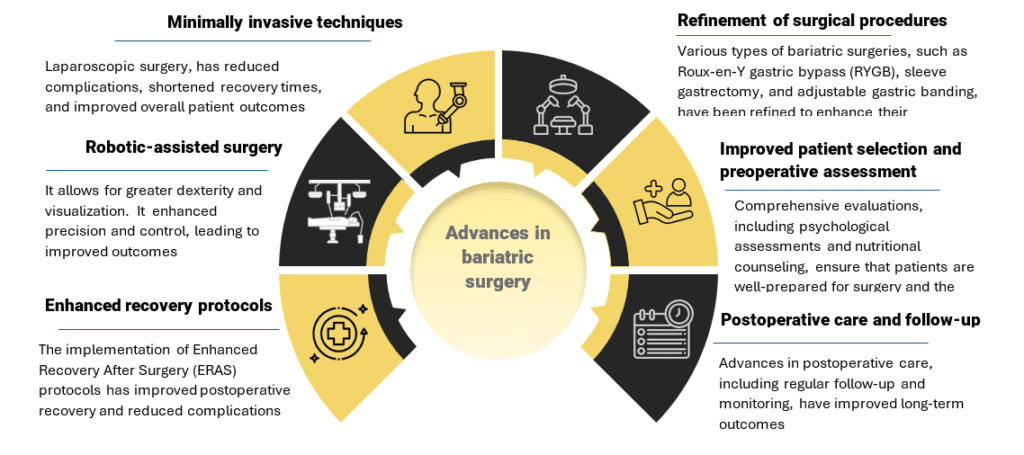
Bariatric surgery has evolved significantly over the years, with advances in surgical techniques leading to improved safety profiles and better patient outcomes.
Key advancements in bariatric surgery
4.4. Lifestyle and behavioral interventions
Technological innovations have transformed support for lifestyle changes in type 2 diabetes management, leveraging digital health platforms, mobile apps, wearable devices, AI, machine learning, and telemedicine. Integrated approaches address the crucial role of mental and behavioral health in managing diabetes through counseling, mindfulness programs, peer support networks, integrated care teams, motivational interviewing, digital cognitive-behavioral interventions, and education. These advancements in lifestyle and behavioral interventions, coupled with integrated care strategies, promise improved patient outcomes and quality of life by comprehensively addressing both physical and psychological aspects of diabetes management.
5. Pipeline developments ushering in a new era
The diabetes treatment pipeline is witnessing groundbreaking advancements that hold the promise of transforming diabetes care. For type 1 diabetes, beta-cell replacement and immunotherapy are paving the way towards potential cures. For type 2 diabetes, novel glucose-lowering medications and bariatric surgery offer effective options for glycemic control and complication prevention. As these therapies continue to develop and undergo rigorous clinical testing, they bring hope for better management and improved quality of life for individuals living with diabetes.
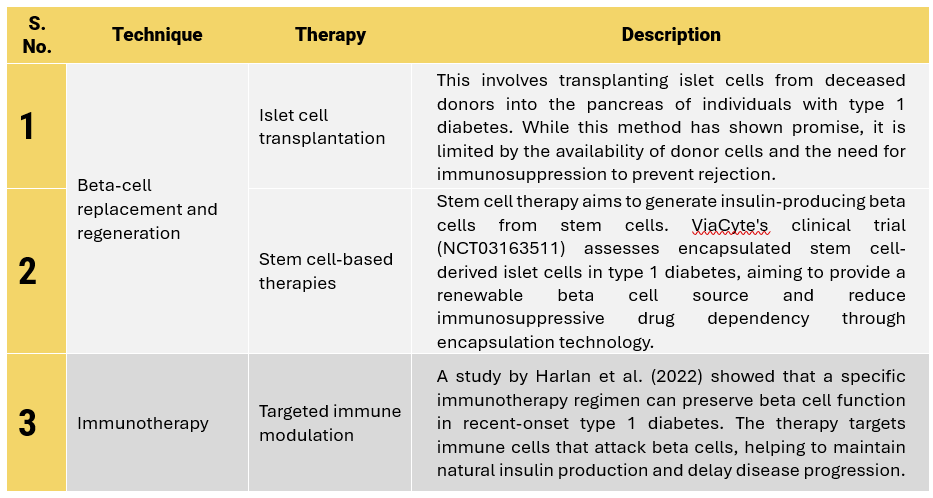
Pipeline developments for the treatment of type 1 diabetes:
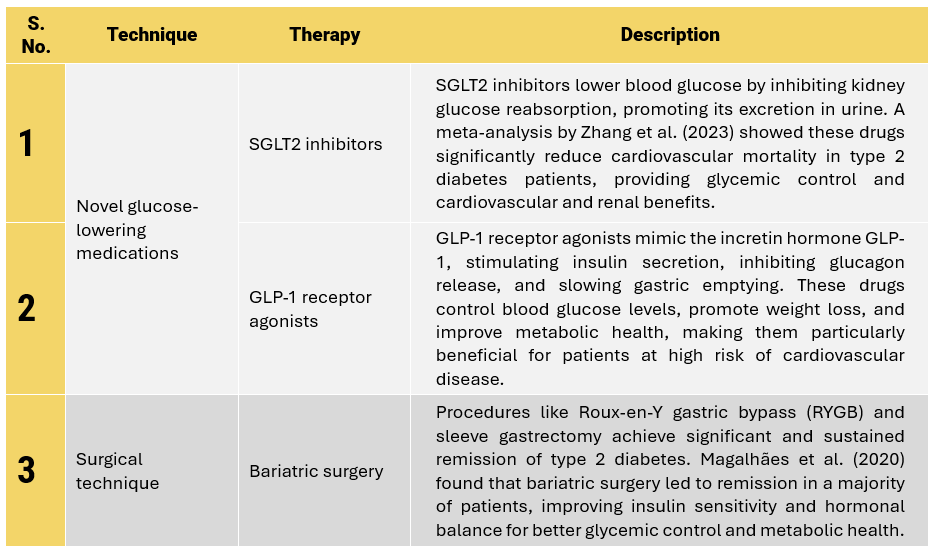
Pipeline developments for the treatment of type 2 diabetes:
These advancements represent a significant leap forward in the fight against diabetes, promising not only to improve the quality of life for individuals living with the disease but also to potentially alter its course. As these therapies continue to develop and undergo rigorous clinical testing, the future of diabetes care looks increasingly hopeful, offering better management strategies and the possibility of long-term remission or even cures. The continued innovation and research in this field underscore a commitment to tackling one of the most prevalent and challenging health issues of our time.


